Medicare Will Cover Telehealth: Medicare will continue to cover telehealth through January 30, 2026, thanks to a last-minute extension passed in response to the 2025 federal government shutdown. This development impacts millions of Medicare beneficiaries, thousands of healthcare providers, and the overall accessibility of care across the United States. Let’s break it down in plain talk — what happened, what’s covered now, what’s changing later, and how you can actually use this information to your advantage whether you’re a patient, provider, or policymaker. We’ll also dig into data, real-life examples, and what the future might hold for virtual care.
Table of Contents
Medicare Will Cover Telehealth
Medicare’s telehealth coverage extension through January 30, 2026 brings stability, clarity, and access to millions of people who depend on virtual care. Whether you’re managing chronic illness, seeking mental health support, or just need a quick check-up — you can keep doing it from the safety and comfort of home. But the clock is ticking. Without further legislation, these flexibilities expire in early 2026. That’s why patients, providers, and policymakers need to keep this issue front and center. The future of healthcare is already here — we just have to make sure the rules catch up.
| Topic | Details |
|---|---|
| Telehealth Coverage Extended Through | January 30, 2026 (pandemic-era flexibilities reinstated) |
| Where You Can Use Telehealth | Anywhere in the U.S., including at home |
| Eligible Providers | Includes doctors, nurse practitioners, therapists, behavioral health providers, FQHCs, RHCs |
| Audio‑Only Telehealth | Still covered for many services |
| Retroactive Claims | Services rendered between Oct 1, 2025 – Jan 30, 2026 can be reimbursed |
| Post-Extension Uncertainty | Old geographic/originating-site restrictions could return after Jan 30, 2026 |
| Official Source | Medicare.gov |
What Prompted This Medicare Will Cover Telehealth Extension?
Back in 2020 when COVID-19 shut everything down, Congress temporarily loosened Medicare’s historically strict rules on telehealth. Before that, Medicare only covered telehealth if you lived in a designated rural area and visited a healthcare facility to connect with a doctor remotely.
But the pandemic changed everything. Congress expanded telehealth coverage through temporary waivers, which allowed Medicare beneficiaries to receive care from the comfort of home — regardless of location. These changes helped more than 28 million beneficiaries maintain access to care, especially those with chronic conditions or mental health needs.
Fast forward to October 1, 2025: the federal government entered a record-setting 43-day shutdown, causing many of those temporary flexibilities to expire. Suddenly, Medicare providers were unsure whether virtual visits would be reimbursed. Some patients were denied coverage. Providers paused scheduling telehealth services altogether.
Fortunately, Congress stepped in before things got worse. A continuing resolution passed in November 2025 retroactively reinstated Medicare’s telehealth flexibilities and extended them through January 30, 2026. CMS (Centers for Medicare & Medicaid Services) confirmed that services delivered during the shutdown window can be re-billed and reimbursed under the updated policy.
What Medicare Telehealth Covers — Through January 2026
With the extension, the expanded telehealth coverage is back — and here’s what that looks like:
1. You Can Get Telehealth Anywhere in the U.S.
Whether you live in a rural area, a city, or somewhere in between, geographic restrictions are waived. You don’t need to go to a clinic to access services. You can do a virtual visit from your bedroom, front porch, or even your grandchild’s living room.
2. No In-Person Requirement for Most Visits
Many services — such as general checkups, chronic condition management, mental health care, and counseling — do not require an in-person visit before or after a telehealth appointment.
3. Audio-Only Appointments Are Covered
Not everyone has access to video-capable devices or high-speed internet. Medicare continues to cover audio-only telehealth visits for many services — including mental health counseling and certain medical evaluations. This ensures older adults and people in underserved areas aren’t left behind.
4. More Providers Can Bill Medicare
As part of the waiver extension, the list of eligible providers includes:
- Physicians
- Nurse practitioners
- Physician assistants
- Clinical psychologists
- Physical, occupational, and speech therapists
- Licensed clinical social workers
- Audiologists
- Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs)
This means more flexibility for clinics, therapists, and specialists to provide services and get paid fairly.
5. Reimbursement for Past Services
If your provider delivered a telehealth service during the shutdown period (Oct 1–Nov 12, 2025) but was denied reimbursement, they can now resubmit those claims. CMS will honor and pay eligible claims under the extended policy.
Why Medicare Will Cover Telehealth Matters for Everyday Americans?
Telehealth isn’t just a convenience — for many, it’s a lifeline. Consider these real-world examples:
- Betty, a retired schoolteacher in Kansas, lives 40 miles from the nearest specialist. With telehealth, she doesn’t have to travel in bad weather or pay for gas just to manage her diabetes.
- Tyrone, a Navy veteran in Detroit, struggles with PTSD. He attends weekly counseling sessions via phone because his smartphone doesn’t support video.
- Maria, a bilingual home health aide in California, helps her elderly clients connect with virtual doctors in both English and Spanish — from their kitchen tables.
These are just a few examples of how telehealth breaks down barriers to care — especially for the elderly, rural populations, and those with disabilities.
Practical Advice for Medicare Patients
Here’s what beneficiaries should know and do:
Don’t Delay Care
If you’ve been putting off appointments due to confusion around coverage — now’s the time to get back on track. Whether it’s managing blood pressure, checking labs, or attending therapy, telehealth is available and reimbursed.
Ask About Audio-Only Options
If you don’t have a smartphone or tablet, ask your provider if a telephone-only visit is appropriate for your care. These are often covered and effective for follow-ups, chronic condition management, and mental health visits.
Keep Track of Denied Claims
If you or your provider received a denial between October and November 2025, call them and ask about reprocessing the claim. Medicare has instructed providers to re-bill for those services under the reinstated flexibilities.
What Happens After January 30, 2026?
Here’s the deal — if Congress doesn’t act again, the telehealth rules snap back to the pre-pandemic model. That means:
- You may need to be in a rural area and go to a medical facility for telehealth services to be covered.
- Audio-only visits may no longer be covered in most cases.
- Fewer types of providers will be allowed to offer telehealth through Medicare.
- Mental health care rules could become more restrictive.
Several bills have been introduced to permanently expand Medicare telehealth — including the Telehealth Expansion Act and the CONNECT for Health Act — but none have passed both chambers as of now.
What Providers Should Know and Do?
If you’re a physician, therapist, or health system administrator, this extension means:
Review Claims from the Shutdown Period
CMS has made it clear that services provided during the lapse (Oct–Nov 2025) are eligible for reimbursement. If you paused telehealth billing, revisit your records and submit corrected claims.
Train Billing Staff
Keep your administrative and coding staff updated on the latest guidance from CMS. The place-of-service code, modifiers, and documentation standards may vary by service type.
Plan for Possible Rollback
Unless Congress passes permanent legislation, you’ll need to be ready for a reversion to pre-2020 rules. This could impact workflows, technology use, and staffing models. Planning now can reduce disruption later.
Looking at the Bigger Picture: The Future of Virtual Care
In many ways, the 2020s have proven that virtual care is not a temporary patch — it’s a permanent pillar of healthcare.
According to the American Medical Association, over 70% of physicians now use telehealth weekly. Mental health professionals have reported increased engagement and reduced no-show rates when using video or phone visits.
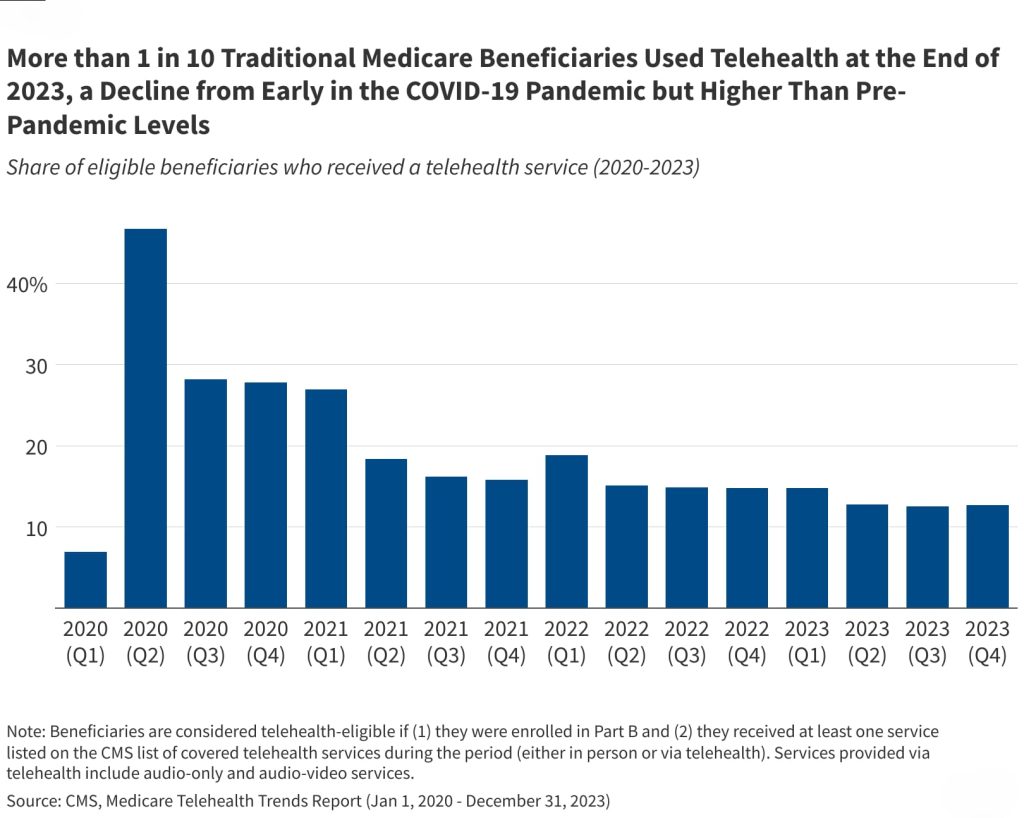
From 2020 to 2024, the number of telehealth claims jumped by more than 4,000%, then stabilized at more than 20x pre-COVID levels.
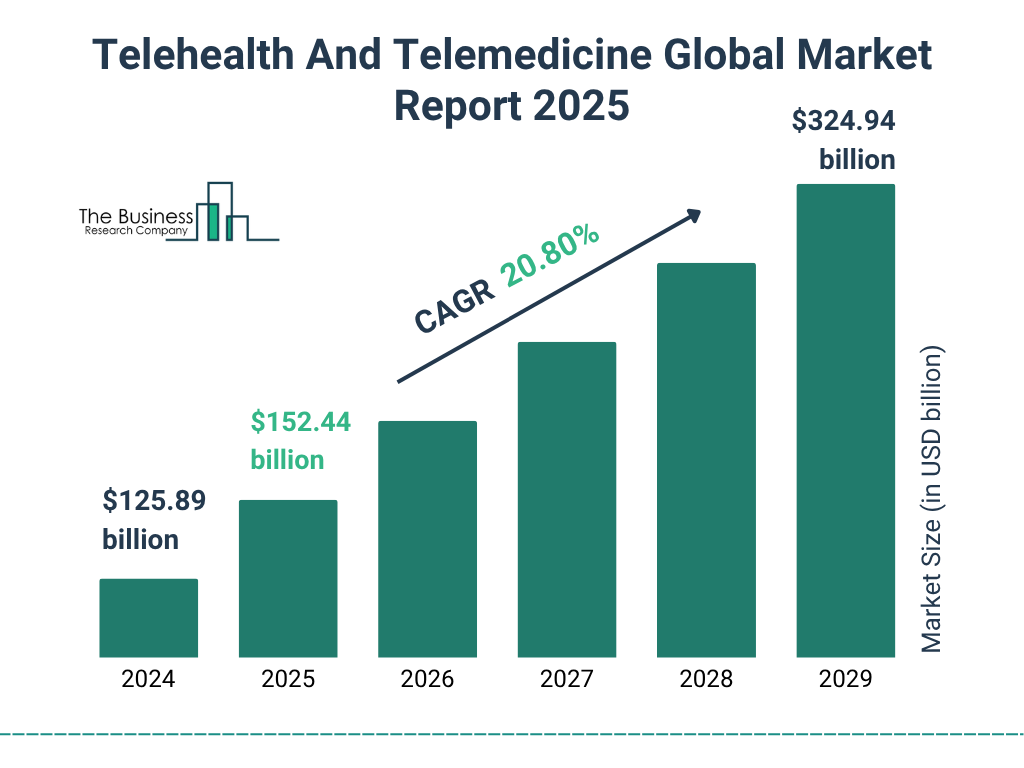
In 2026, the market for remote monitoring and virtual care is projected to exceed $175 billion. (drkumo.com)
And let’s not forget that telehealth improves equity. For many Native communities, Black and Latino patients, people with disabilities, and those living in poverty — virtual care is often the only viable path to consistent health services.
VA Disability Benefits January 2026 – Updated Payment Levels, Deposit Dates, and Eligibility
Medicare Update 2026: Some Prescription Drug Costs Expected to Drop by Half
2026 Social Security Update: Check Important Changes to COLA, Medicare Costs, and Benefit Rules