Medicaid in 2026: Medicaid in 2026 is rolling through some of its biggest changes since the Affordable Care Act expanded it back in 2010. If you or someone in your family gets Medicaid—or might qualify soon—now’s the time to get the facts straight. This article covers everything you need to know: new federal rules, work requirements, rural health investments, drug pricing reforms, eligibility changes, and how you can prepare to protect your healthcare coverage. Whether you’re a busy parent, a college student trying to understand new rules, or a healthcare professional advising patients, you’ll find practical, easy-to-follow insights right here.
Table of Contents
Medicaid in 2026
Medicaid in 2026 isn’t disappearing—it’s just changing shape. For millions of Americans, it still provides lifesaving, affordable care. But the new rules—like work requirements and more frequent eligibility checks—mean it’s not automatic anymore. If you stay proactive, know your rights, and keep your paperwork straight, Medicaid can still be a reliable, steady source of healthcare security for you and your family.

| Category | Update in 2026 | Why It Matters |
|---|---|---|
| Work/Engagement Rules | 80 hours/month required for some adults | New eligibility condition with reporting |
| Eligibility Verifications | Every 6 months | More frequent paperwork needed |
| Enrollment | Flat 0.2% projected growth | COVID-19 continuous enrollment ended |
| Spending Growth | +7.9% expected in FY2026 | Driven by drugs, long-term care |
| Drug Pricing | Generous Model launches | States may pay less for meds |
| Rural Health Funding | $147M+ per state | Expands access in rural clinics |
| Immigrant Eligibility Limits | Tighter restrictions in some categories | Reduces coverage for some non-citizens |
| Provider Funding Cutbacks | Planned Parenthood blocked in 22 states | Reduced access in some areas |
What Is Medicaid in 2026 and Why Does It Matter?
Medicaid is the largest public health insurance program in the U.S., serving more than 85 million Americans as of 2025. It covers low-income families, seniors, people with disabilities, pregnant women, and children—with services ranging from hospital visits and prescriptions to home care and behavioral health.
What makes Medicaid unique is that it’s jointly run by the federal government and individual states, which means rules can vary depending on where you live. It’s also means-tested, meaning your eligibility is tied to your household income and situation.
In 2026, Medicaid is evolving to reflect new policies aimed at encouraging work, reducing fraud, cutting costs, and expanding services in under-served areas.
What’s Changing in Medicaid in 2026?
Let’s break down each major shift and what it means for you and your family.
1. Work and Community Engagement Requirements
For the first time in a decade, the federal government is allowing states to require that some adult Medicaid recipients prove they’re working or doing community service to keep their coverage.
What’s Required?
If you’re between 19 and 64 years old, not pregnant, and don’t have a disability, your state may require that you:
- Work at least 80 hours a month
- Be enrolled in school or job training
- Volunteer for community service
- Or combine all of the above
This rule doesn’t apply to everyone, and most states must provide exemptions for:
- Parents caring for young children
- People who are medically frail
- Individuals in recovery programs
- Those facing significant barriers to employment
Important: States like Arkansas, Kentucky, and Georgia are preparing to implement these requirements in phases by the end of 2026 or early 2027.
Documentation will be required—often through online portals, monthly logs, or reporting by employers or community organizations.
2. Semi-Annual Eligibility Checks
Historically, Medicaid eligibility was checked once per year. Now, states will begin verifying income and household changes every six months, making it easier for people to lose coverage due to paperwork issues.
What to Expect:
- Renewal packets sent twice a year
- Required proof of income, residency, household members
- Loss of coverage for missing a deadline
To avoid surprises, keep your address and contact info updated with your state Medicaid office. And set reminders to reverify your details before your renewal date.
3. Slowing Enrollment, Growing Costs
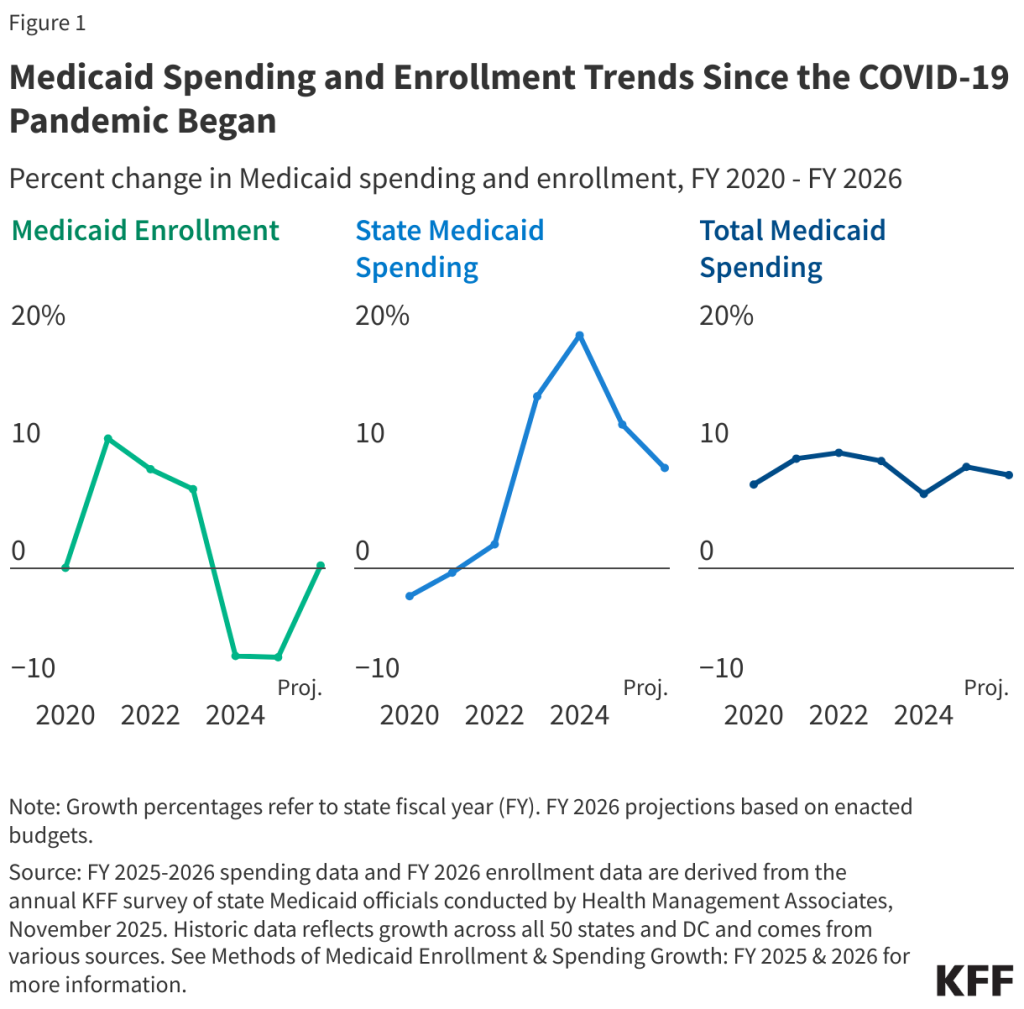
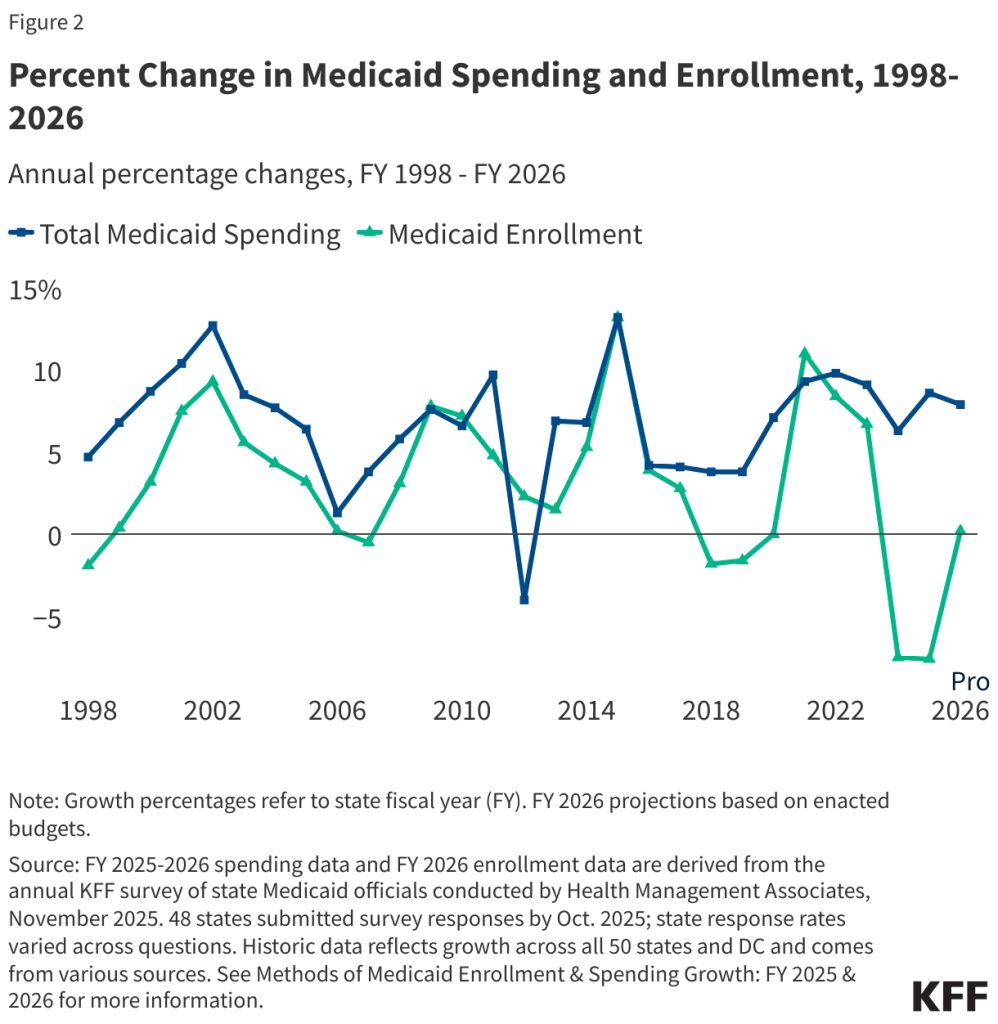
Medicaid enrollment soared during COVID-19 because of rules that prevented disenrollment. But in 2026:
- Enrollment is expected to grow just 0.2%, according to KFF
- Medicaid spending is expected to grow nearly 8%, driven by:
- Higher drug prices
- Aging populations
- More long-term care needs
- Behavioral health and substance abuse treatment
Even though fewer people are enrolling, each enrollee is costing more to cover—leading states to rethink benefits, provider payments, and budget sustainability.
4. Rural Health Boost: $147M+ Per State
The federal government is tackling rural healthcare disparities with a massive cash infusion:
- Over $147 million per state to build rural health infrastructure
- Investments in:
- Telemedicine
- Community clinics
- Transportation for medical visits
- Broadband for remote areas
For families in remote or medically underserved areas, this could mean new clinics, better tech, and easier access to specialists.
5. New Drug Pricing Program (“Generous Model”)
The U.S. is launching a voluntary pricing program that allows states to negotiate lower prices for medications by referencing the prices paid in other wealthy nations like:
- Canada
- Germany
- Australia
If your state opts in, you could start seeing lower co-pays or state spending on prescriptions, especially for costly medications like insulin or cancer therapies.
6. Coverage Changes for Immigrant Populations
Some immigration categories will lose Medicaid access in 2026 due to tightened eligibility rules under the One Big Beautiful Bill Act.
Groups potentially affected include:
- Asylum seekers in pending status
- Humanitarian parolees
- Refugees who haven’t passed the 5-year residency mark
If you’re an immigrant or mixed-status family, it’s essential to check updated state eligibility charts or consult immigration-focused legal aid groups.
7. Cuts to Planned Parenthood and Some Providers
A court ruling now allows the federal government to withhold Medicaid funding from Planned Parenthood and certain other providers in 22 states, starting in 2026. This means:
- Reduced access to family planning services
- Fewer providers offering free or low-cost STI testing
- Potential gaps in preventive care like Pap smears and breast cancer screenings
In response, advocacy groups and some states are working on state-level funding workarounds to maintain access.
What Benefits Are Still Covered in Medicaid in 2026?
Despite the changes, Medicaid still covers a broad list of essential health benefits, including:
- Doctor and hospital visits
- Emergency care
- Prescription medications
- Dental and vision (in some states)
- Mental health and substance use treatment
- Home- and community-based services
- Preventive care and screenings
- Long-term care for elderly and disabled populations
Children, pregnant people, and people with disabilities are strongly protected under federal law, and states must continue to provide robust care for these groups.
What This Means for You and Your Family?
Let’s take some everyday examples.
Example 1 – A Young Adult with a Part-Time Job
Alex, 27, works 15 hours a week and volunteers at a local food pantry. If Alex lives in a state with new engagement rules, they may need to report those 60+20=80 hours to keep coverage.
Example 2 – A Grandmother Caring for Grandkids
Gloria, 61, is on Medicaid and caring for her toddler grandson full-time. She may be exempt from new work rules and should notify the state of her caregiver role.
Example 3 – A College Student on Medicaid
Jordan, 20, is enrolled in a community college and qualifies for Medicaid. They may meet work/engagement requirements just through full-time coursework.
Medicare Update 2026: Some Prescription Drug Costs Expected to Drop by Half
It’s Official: Medicare Will Cover Telehealth Through January 2026 Amid Federal Shutdown Fallout
When is the January 2026 Florida TCA Payment made? Check Eligibility
How to Stay Covered in 2026 – Action Steps
- Update Your Info: Go to your state Medicaid portal and confirm your mailing address, income, and contact details.
- Watch for Mail: Renewal forms and eligibility verifications will come by mail or email. Don’t toss them!
- Ask Questions: Talk to a Medicaid navigator, case worker, or community health center for free help.
- Document Activities: If you’re working or volunteering, save pay stubs, logs, or class schedules.
- Appeal if Dropped: If you’re dropped in error, you can appeal or request a fair hearing within 30–90 days.