House GOP’s New Health Plan: In December 2025, the House Republicans unveiled a new health care proposal that’s sparking intense debate from lawmakers, health policy experts, and American families alike. The headline that caught everyone’s attention? The GOP plan does not include an extension of Affordable Care Act (ACA) premium subsidies, which are set to expire at the end of 2025.
These subsidies have helped millions of Americans afford health insurance under the ACA — also known as Obamacare. Without them, premiums for many people could rise dramatically in 2026. That has real-life consequences for working families, small businesses, and even local economies. But the GOP leadership is standing firm, arguing that extending the subsidies isn’t the right way to fix health care. In this article, we’ll break down exactly what the GOP’s health plan includes, why the subsidies are being left out, and what this means for Americans heading into 2026. Whether you’re a policy analyst, small business owner, or just trying to understand your own health care options, this is your guide.
Table of Contents
House GOP’s New Health Plan
The House GOP’s new health plan represents a sharp turn in the health care policy debate. By excluding the continuation of ACA premium subsidies, Republicans are signaling a clear intent to move away from Obamacare-era programs and toward a more market-driven approach. But the cost of that decision could be steep — not just in political terms, but in the lives and wallets of millions of Americans. The debate over how we fund health insurance in this country is far from over, and the stakes couldn’t be higher. As the clock ticks toward the subsidy expiration date at the end of 2025, Americans across income levels are watching closely — and preparing for a potentially more expensive year ahead.

| Topic | Details | Impact |
|---|---|---|
| House GOP Plan | A new health proposal with reforms on insurance access, pharmacy transparency, and cost-sharing | Targets market reforms but excludes premium subsidies |
| ACA Subsidies | Enhanced tax credits that reduce health insurance costs for millions | Set to expire Dec. 31, 2025 |
| Impact of Expiration | Millions may face much higher premiums in 2026 | Potential drop in coverage, increase in uninsured rates |
| Political Divide | GOP sees subsidies as unsustainable and anti-market | Democrats argue they’re essential for affordability |
| Coverage Risk | CBO estimates millions could lose insurance without subsidy extensions | Coverage gap likely to widen among middle-income Americans |
What’s Actually in the House GOP’s New Health Plan?
The House Republican plan includes a few major policy initiatives aimed at reducing the cost of health care by increasing competition and transparency. But it stops short of major structural reforms or introducing new sources of coverage funding.
Here are the key components:
1. Expansion of Association Health Plans (AHPs)
The plan promotes Association Health Plans, which allow small businesses and self-employed individuals to band together to purchase insurance as a group. The goal is to provide cheaper premiums by pooling risk across a larger group.
However, critics argue that these plans can weaken consumer protections and exclude individuals with preexisting conditions, because they are often not required to follow ACA coverage standards.
2. Pharmacy Benefit Manager (PBM) Transparency
Another key feature of the GOP plan is increasing transparency in the prescription drug supply chain. Specifically, it focuses on the role of pharmacy benefit managers — middlemen who negotiate drug prices between insurers and manufacturers. The GOP wants PBMs to disclose how much money they keep and how much is passed on to consumers.
This is widely supported across party lines, as drug costs are a major driver of overall health spending. But while it addresses a legitimate issue, it doesn’t directly help with premium affordability.
3. Cost-Sharing Reductions for Some Consumers
The GOP plan includes temporary funding to reduce out-of-pocket costs — things like copays and deductibles — for certain low-income enrollees. While helpful for those who qualify, these changes are narrowly targeted and don’t address the bigger affordability crisis facing the broader middle class if subsidies vanish.
What’s Not in the Plan: ACA Subsidy Extensions
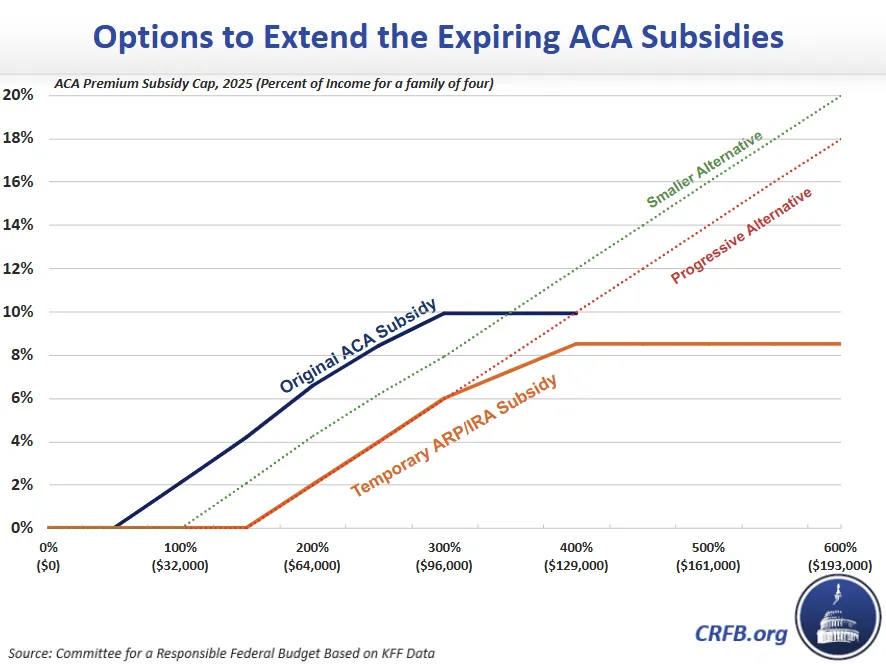
The enhanced ACA premium subsidies, which were first expanded under the American Rescue Plan Act of 2021 and extended through 2025 by the Inflation Reduction Act, are not included in the House GOP’s health bill.
These subsidies currently provide crucial tax credits to more than 20 million Americans, dramatically lowering the cost of monthly premiums for marketplace plans. They are income-based and were designed to ensure that no one pays more than 8.5% of their household income on health insurance premiums.
If these subsidies are allowed to expire:
- A 45-year-old earning $45,000 could see monthly premiums rise from $110 to over $450.
- A family of four earning $80,000 could face a $600+ monthly increase in premium costs.
- Seniors and early retirees on ACA plans would be particularly hard-hit due to age-based pricing.
This isn’t just about politics — it’s about affordability for working Americans.
Why Aren’t the Subsidies Included in the House GOP’s New Health Plan?
House Republicans have offered several reasons for excluding the subsidy extensions from their 2025 health plan:
1. Ideological Differences
GOP lawmakers view ACA subsidies as part of a system they’ve long opposed. To many Republicans, continuing the subsidies would signal an acceptance — or even an endorsement — of Obamacare, a law they’ve repeatedly tried to repeal.
They argue that government subsidies distort the market, discourage private-sector competition, and create long-term fiscal liabilities.
2. Focus on Market-Based Reforms
Instead of direct government subsidies, GOP leaders prefer solutions like:
- Expanding Health Savings Accounts (HSAs)
- Encouraging private insurance competition
- Supporting small businesses in accessing group plans
They believe these reforms offer a more sustainable way to improve access and lower costs.
3. Strategic Political Calculations
Extending subsidies now would require bipartisan negotiation — and possibly compromise on other GOP priorities. By excluding the subsidies, House Republicans are drawing a line in the sand and using the issue as a potential bargaining chip in broader budget talks.
Some within the party may also be aiming to avoid giving Democrats a “win” ahead of the 2026 midterm election cycle.
Economic & Health Impact of Expiring Subsidies
The consequences of allowing ACA subsidies to expire are significant — and measurable.
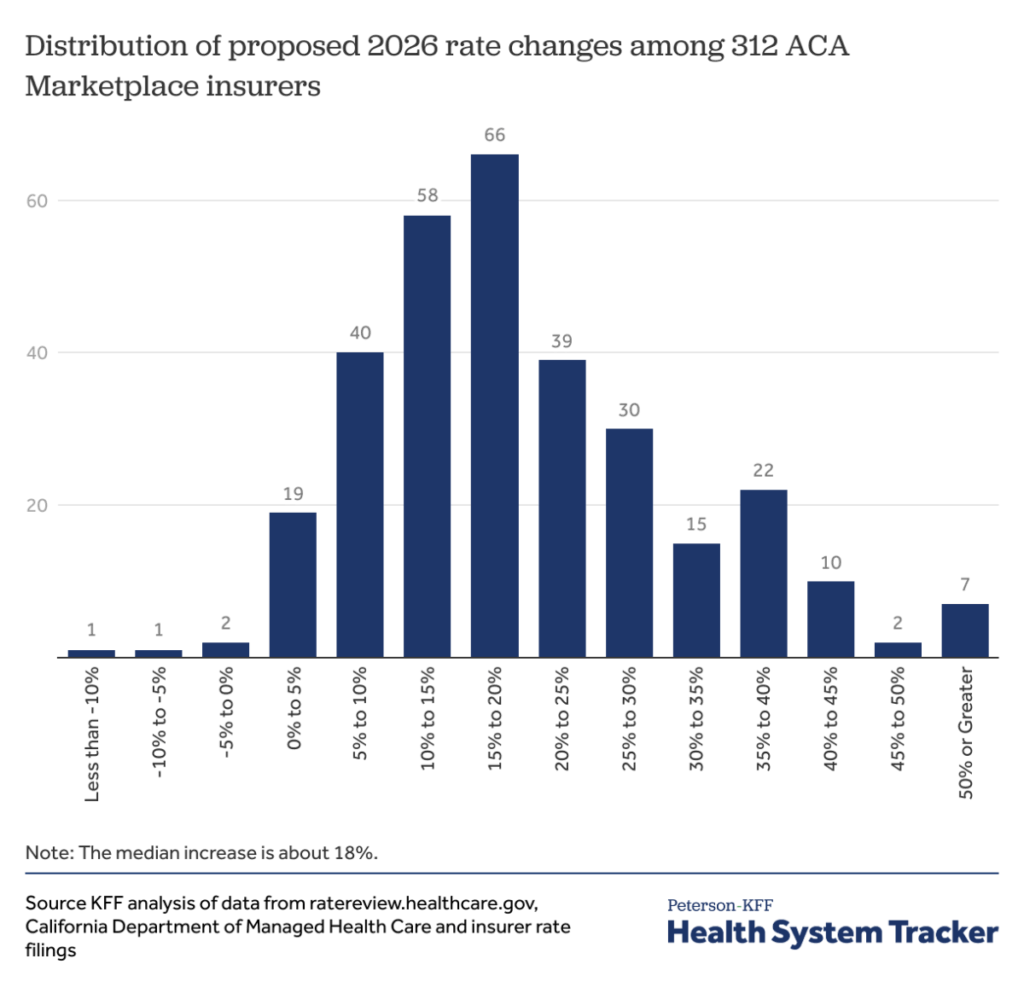
1. Premium Increases
According to recent projections by the nonpartisan Congressional Budget Office (CBO), premiums for marketplace plans could rise by 40% to 90% for many enrollees in 2026. That’s a devastating increase for middle-income Americans who don’t qualify for Medicaid and don’t get insurance through their employer.
A family earning $70,000 per year could see their premiums increase by over $7,000 annually without the subsidies.
2. Coverage Loss
CBO estimates show that 3 to 7 million people may lose insurance coverage altogether if the enhanced subsidies disappear. Many more may switch to lower-quality, high-deductible plans or go without coverage until they face an emergency.
This could reverse more than a decade of progress under the ACA in reducing the uninsured rate, especially in rural states and among working-class adults.
3. Broader Economic Ripple Effects
Research from the Commonwealth Fund suggests that expiring subsidies could also lead to job losses in the health care industry. Fewer insured patients means fewer appointments, fewer procedures, and less revenue for hospitals, clinics, and providers. That would directly impact employment in health care — one of the largest sectors in the U.S. economy.
The Medicaid Connection
In many states, Medicaid expansion under the ACA has helped reduce uninsured rates among the poorest populations. But in states that chose not to expand Medicaid, ACA marketplace subsidies are the only affordable option for many low-income adults.
If those subsidies disappear, people in non-expansion states — often in the South — could face a complete coverage gap. They’d earn too much for Medicaid, but not enough to afford unsubsidized private insurance.
This would leave millions caught in what policy experts call the “coverage gap,” a scenario the ACA was explicitly designed to prevent.
The Political Divide — And a Deepening Gridlock
The current stalemate over subsidies isn’t just a technical budget issue — it’s a battle over the role of government in American health care.
Democrats want to permanently extend the subsidies and, in some cases, expand them further. They view health care as a public good and argue that government support is necessary to ensure affordability and equity.
Republicans believe that market competition and personal responsibility are better solutions. They’re wary of expanding entitlements and see ACA subsidies as part of a larger pattern of government overreach.
This ideological divide makes compromise difficult — especially in an election year.
House GOP’s New Health Plan: What Happens Next
There’s still a chance that Congress could extend the subsidies through a separate legislative vehicle in 2026. Some bipartisan lawmakers are working on proposals to do just that. But timing is critical.
If Congress waits until the second half of 2026, insurance companies may already have filed new, higher premiums for the year. That means some Americans may be priced out of the market even if subsidies are later restored.
Health policy experts are urging swift action to provide certainty — for insurers, consumers, and state regulators.
Congress Considers Issuing New Social Security Numbers — Here’s What the Proposal Includes
How nonprofit lenders could save you thousands on student loans
$500 a Month, No Strings Attached; Are You Eligible for America’s First Guaranteed Income Program?